How does hospital funding affect treatment?
Healthcare is something that is non-negotiable for all people. Whether it be for a cold or for a chronic illness, we all in some way depend on aspects of the healthcare industry, making it a basic human necessity. However, like most industries in our society, healthcare has become a business – a business whose primary focus is to maximize profits, therefore the cost is always passed on to the consumer. In this case, the consumer is the patient. This raises the question on whether or not the healthcare industry’s focus on profits comes at the expense of the patient and affects their outcomes/treatments in a negative way.
Funding Sources
It is a well known fact that healthcare funding typically comes from three places: government programs (Medicare, Medicaid), private insurers, and individual patients. It is also a known fact that the US spends quite a lot on healthcare, as there is more money spent than other developed countries, including countries that provide universal healthcare.
In 2018, the U.S spent 16.9% of its gross domestic product (GDP) on healthcare, which is almost twice as much as countries like Australia and the U.K that spend 9.3% and 9.8% of their’s on healthcare (U.S. Health Care From a Global Perspective, 2019: Higher Spending, Worse Outcomes?, 2020). But just because the US is spending a lot of money on healthcare does not necessarily mean that its citizens are benefitting. In fact, American citizens are suffering at the hands of the healthcare industry.
Profits Over Patients
The first element of proof that the healthcare industry is more concerned with profits than patients – leading to negative outcomes for the patients – is found within the organizational structure and funding structures of hospitals, the very institutions that are supposed to administer healthcare services to individuals. Hospitals take one of two forms. They are either a “nonprofit” or a “for profit” entity. The primary difference between these two is, of course, that the former is meant to accrue institutional value while the latter doesn’t (instead relying on the fact they do not have to pay any taxes in order to create financial benefit for the organization.) However, that does not mean that nonprofit hospitals are devoid of revenues. In fact, nonprofits receive funding in various ways ranging from charities to religious organizations to grants, all while maintaining their tax exempt status under the guise of returning charitable care services to their communities.
It is well documented that nonprofits spend their money on things other than care within the community. Dr. Elisabeth Rosenthal, in her book “An American Sickness”, states, “1A survey of the forms conducted by the California Nurses Association concluded that 196 hospitals received ‘$3.3 billion state and federal tax exemptions and spent only $1.4 billion on charity care – a gap of $1.9 billion” (2017, 50)). This is a truly disturbing trend, if you consider that hospitals – whose primary purpose is to care for individuals in their community – are benefiting financially from diverting more than 50% of their funding to elements other than patient care, which diminishes the patient experience and creates negative outcomes for those individuals.
One would think that due to the ability of for-profits to charge more without the duty to the community that nonprofits have that they would be known for providing better care and treatment to its patients than their community-based counterparts. However, this is not the case. According to the University of Southern California (USC, 2022), while for-profits charge more for services than nonprofits, they are known to be worse in terms of treating even common illnesses, and they hold higher death rates. This becomes a problem for the low income individuals seeking healthcare, because as stated previously non-profits (who are cheaper and cannot turn away someone who need care regardless of their ability to pay) are typically set up in richer areas, and for-profits can be usually found in lower income communities. But regardless of where patients fall on the socio-economic scale, they take a backseat to revenues (from the perspective of the hospitals), receiving compromised care and negative outcomes.
Healthcare: A Profitable Business
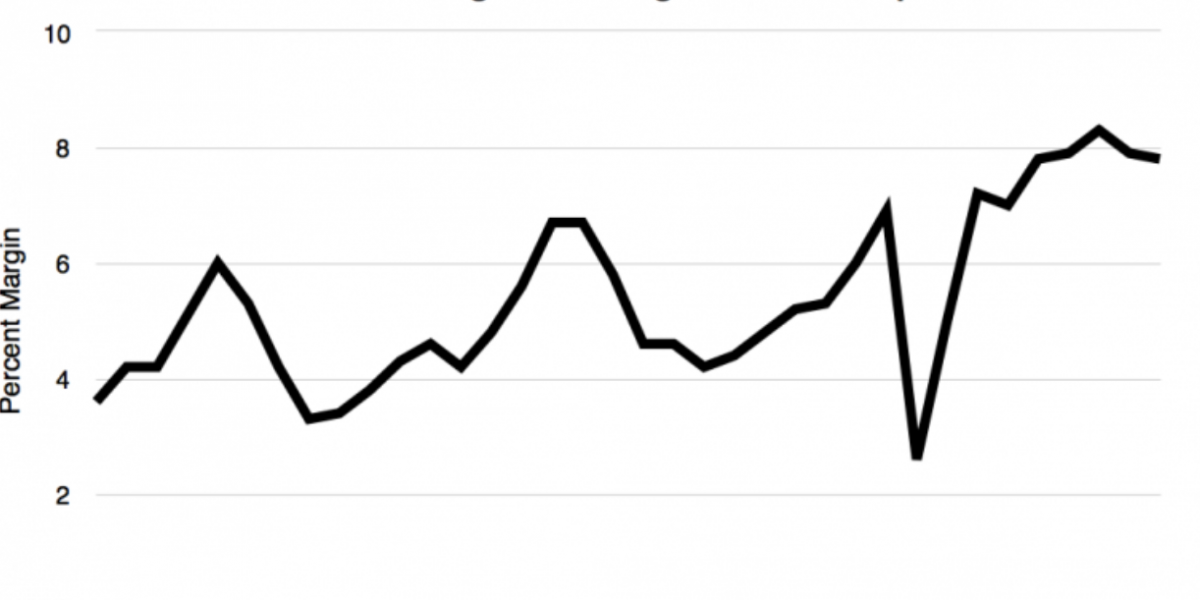
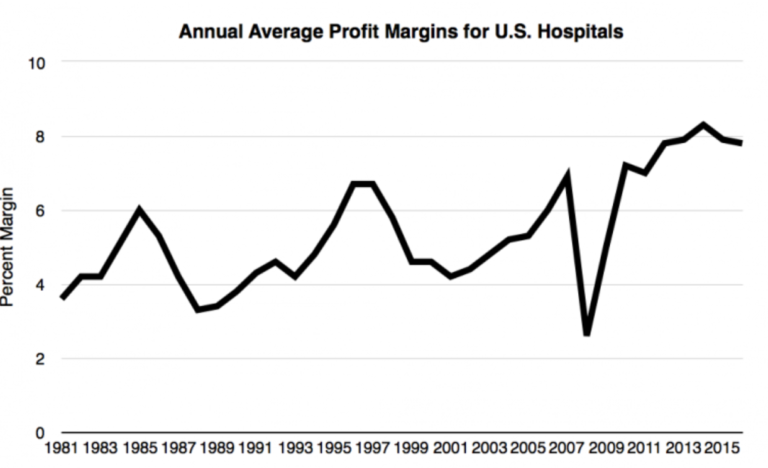
The figures below show the annual profit margins of American hospitals from 1981 to 2016. As you can see, there has been a steady increase throughout the years, with the exception of 2008 (when the U.S. economy was in a recession).
For those who champion the perspective that the way to close this gap in health outcomes is simply for the government to subsidize patient care, consider this: according to Urban.org, in 2019 $322 billion was spent on healthcare and hospitals by local and state governments. These figures do not include the amount that the federal government contributes via Medicare and Medicaid, as they are considered public welfare contributions. Therefore, between local, state, and federal funding, the US has more than enough government funding to properly care for its patients and ensure equitable health outcomes for its citizens. If countries like Switzerland can spend the equivalent of $88.25 billion, while providing universal health care to its citizens, then the US should not be spending this much while having so many people who cannot afford healthcare.
Funding Sources vs. Quality of Care
With all of the money being spent on healthcare in America, why are we not seeing better results in healthcare for everyone? I think the answer lies in the way that patients react to the current healthcare system, which is neither patient-centric nor transparent. The 2018 Hospital Patient survey from Scorpion.co showed that out of 1000 healthcare patients the majority preferred being aware of what insurances were accepted prior to the meeting. In addition, they value education and training, compassionate care, and strong communication skills in doctors. However, this information is not always readily available for patients seeking access to the healthcare system.
Other things that might influence a consumer’s decisions are the service quality, wait times, proximity and cleanliness. I conducted an interview with my own father to see what was behind his decisions regarding healthcare providers. His primary concern was how good the healthcare would be, along with overall convenience. While there are several health facilities nearby that he could have chosen, he picked Walmart Health because the Walmart-brand is known for having low prices. So even though his stated criteria for choosing a healthcare service was “quality” and “convenience”, his ultimate decision was based on the perception of value, even though the prices are not visible until after the doctor visit. But it was obvious to my father that Walmart Health would offer lower prices than other typical doctor’s offices nearby, thus creating the most attractive opportunity for healthcare services.
Looking back on the survey from Scorpion.co, it is apparent that whether a hospital is a nonprofit or for-profit hospital is not a major concern of the patients, (This makes sense, because when was the last time you went to a hospital and sat in a waiting room thinking about how well funded the place is?) However, while hospital funding might not be on the forefront of patients’ minds, funding is responsible for all the things that are important to the patient. All the things that make healthcare facilities impressive to the patient – ranging from high tech machines, to types of treatments available, to the clean and elegant buildings, and the highly trained physicians – are as a result of funding. However, patients are not concerning themselves with the details regarding hospital structure or funding, despite the fact that there is a correlation between the finances of a hospital or healthcare facility and the quality of care and safety. Perhaps they should be concerning themselves with this aspect of their healthcare.
In a 2014 cross-sectional study investigating hospital financial condition and hospital quality and safety at acute care hospitals, it was found that financially stable hospitals are better able to maintain highly reliable systems and provide ongoing resources for quality improvement. We all want the best when it comes to healthcare, so it is unlikely that we wouldn’t prefer to go to the better funded places, and in the cases where we do go to underfunded facilities it is because that is all that is affordable and accessible to us. So while we may not be directly looking at it, funding does play a role in the outcomes patents have.
This also might explain the differences in patient outcomes between non and for profits, which, as we previously discussed, is something funding plays a key role in. It is very easy to see how having better funding would equal better health outcomes. USC Price lists various ways to improve patient outcomes and the answers range from offering tele-health and other technologies, reducing medical errors and increasing patient safety, ensuring continuity of care and discharge procedures.
What's Next?
Since we have acknowledged the issue, we need to identify what the solution would be. Whether it be government support, better planning or a realigning of priorities by healthcare facilities, something needs to be done. Healthcare is something that is an absolute necessity and it is important that that healthcare is efficient and of the best quality, especially in a country that is spending as much as the U.S is on it. Therefore, we need to do a better job at achieving equitable outcomes.
References
U.S. Health Care from a Global Perspective, 2019: Higher Spending, Worse Outcomes? (2020, January 30). Commonwealth Fund. Retrieved March 29, 2022, from https://www.commonwealthfund.org/publications/issue-briefs/2020/jan/us-health-care-global-perspective-2019
Schreck, R. I. (2020, March). Overview of Health Care Financing – Fundamentals. Merck Manuals. Retrieved February 20, 2022, from https://www.merckmanuals.com/home/fundamentals/financial-issues-in-health-care/overview-of-health-care-financing
Carey, M. J. (2020, January 17). How nonprofit hospitals get away with the biggest rip off in America. Medical Economics. Retrieved February 21, 2022, from https://www.medicaleconomics.com/view/how-nonprofit-hospitals-get-away-biggest-rip-america
Rosenthal, E. (2017). An American Sickness: How Healthcare Became Big Business and how You Can Take it Back. Penguin Press.1
Health and Hospital Expenditures. (n.d.). Urban Institute. Retrieved February 21, 2022, from https://www.urban.org/policy-centers/cross-center-initiatives/state-and-local-finance-initiative/state-and-local-backgrounders/health-and-hospital-expenditures=
Health care costs and financing 2019: provisional data. (2021, April 27). Total health expenditure in 2019 at CHF 82.1bn – Health care costs and financing 2019: provisional data | Press release | Federal Statistical Office. Retrieved February 21, 2022, from https://www.bfs.admin.ch/bfs/en/home/statistics/catalogues-databases/press-releases.assetdetail.16306848.html
Hospital Financial Analysis. (n.d.). True Cost of Healthcare. Retrieved February 21, 2022, from https://truecostofhealthcare.org/hospital_financial_analysis/
Survey: How Patients Choose Doctors and Hospitals. (n.d.). Scorpion. Retrieved February 21, 2022, from https://www.scorpion.co/hospitals/expert-tips/intelligence/hospital-patient-survey-how-do-patients-choose-t/
Patient choice modelling: how do patients choose their hospitals? (2017, April 11). PubMed. Retrieved February 21, 2022, from https://pubmed.ncbi.nlm.nih.gov/28401405/
Correlation between hospital finances and quality and safety of patient care. (2019, August 16). PLOS. Retrieved February 21, 2022, from https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0219124
“7 Ways to Improve Patient Outcomes.” Executive Master of Health Administration, https://healthadministrationdegree.usc.edu/blog/7-ways-to-improve-patient-outcomes/. Accessed 4 April 2022.